Pathological Demand Avoidance: A Guide for Parents and Carers

PDA (Pathological Demand Avoidance) is a profile on the autism spectrum, characterised by children who avoid the demands and expectations of everyday life to an extreme extent.
Also known as Extreme Demand Avoidance, PDA commonly presents as highly anxious behaviour and a need for control, especially in unpredictable situations.
While demand avoidance is common in all children, it reaches an all-consuming level in kids living with PDA. Conventional strategies and tools rarely help, leaving parents, carers and educators feeling helpless.
In this post, we explore features of the PDA profile, testing and diagnosis, and the pathway to support.
Living with Pathological Demand Avoidance
Life is a constant battle between fight, flight and freeze for children living with PDA. Unrelenting anxiety drives an obsessive need to resist demands, leading to meltdowns, avoidance, and, at times, extreme behaviour.
Kids with PDA use control, distraction and social strategies to bypass activities they usually enjoy. While this might seem willfully disobedient, meeting demands is out of their control. When PDA takes hold, all suggestions are perceived as demands, and anxiety accelerates.
In a highly anxious state, the brain of a child with PDA is frantically assessing, questioning and buzzing until, eventually, it goes offline and shuts down. When this happens, it’s a matter of can’t complete tasks versus won’t complete tasks.
At its core, PDA is a neurological power struggle between the
DR NICOLE CARVILL
brain, body and heart.
With PDA at play, social interaction, communication and friendships can become tricky, and children need lots of support to manage their emotions.
School, with all its rules and regulations, tends to be a difficult environment for most children with PDA. It’s hard to get to school on time, wear a uniform, follow instructions, socialise, and complete activities, especially if they don’t really interest you. This daily struggle, known as ‘school can’t’, adds pressure and uncertainty at home, impacting the wellbeing of the entire family.
Living with PDA is challenging for children and their family members, but it is not without reward. Kids with PDA tend to be charismatic, tenacious, creative and have a great sense of humour. Their determination and steadfast resolve can be helpful when navigating their way through life.
Behavioural features of PDA
As mentioned, high anxiety is a key component of Pathological Demand Avoidance. When children with PDA feel uncertain or out of control, they instinctively try to take control and may exhibit a number of the following behavioural features:
- An obsessive need for control
- Refusal to cooperate or take part
- Mood fluctuations
- Limited ability to socialise and understand boundaries
- Insisting that others comply with their demands
- A tendency to perceive themselves as an adult and use adult language
- A rich fantasy or role-play world
To alleviate their anxiety and control situations, children with PDA struggle to do the things we take for granted—like putting on shoes and preparing to leave the house. Often, they’ll make elaborate excuses and sabotage situations to avoid participating.
Strategies and coping mechanisms vary between kids and can manifest in different ways. Most commonly, children with PDA:
- Use distraction as a tool to avoid situations or tasks
- May sabotage events or make elaborate excuses to avoid participating
- Can be controlling or dominating, especially during play with other children
- Use frank (and sometimes hurtful) language to control their environment
- Shout, say no or experience a meltdown
- Occasionally, anxiety escalates to aggression or self-harm
For some kids, emotions swing from one extreme to the other.

"PDA is like trying to face your phobias every waking moment!"
– Riko, Riko’s blog.
When distraction, control and avoidance strategies fail, anxiety levels skyrocket, and distress escalates. Adults with PDA sometimes liken this feeling to a panic attack.
The PDA scale of distress
The following illustration provides a sense of how Pathological Demand Avoidance unfolds for most kids.
As you can see, the PDA Scale of Distress begins in a state of calm, escalating to shut down as demands, expectations and anxiety increase.
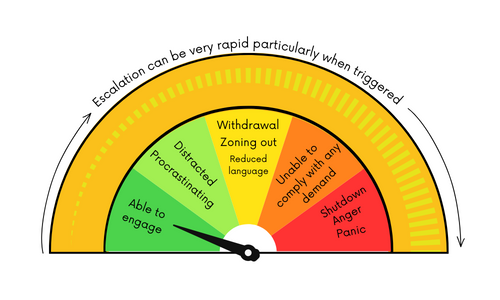
- In the green zones, kids are calm and can engage with those around them but may use distraction and procrastination to avoid demands.
- The yellow zone marks a progression to social withdrawal and a reduced ability to communicate.
- In the orange zone, children with PDA become incapable of meeting demands and expectations.
- The red zone is where the flight, fight or freeze response is activated. Panic, anger and total shutdown are common and kids need extra support to regulate.
Testing for Pathological Demand Avoidance
Health professionals cannot formally diagnose PDA in Australia until the profile is recognised in the global DSM-5 Diagnostic Manual. However, a PDA-aware child psychologist can help you with assessment, profiling and ongoing support.
Your child should have a confirmed Autism Spectrum Disorder diagnosis to be assessed for PDA.
PDA is often misdiagnosed as ODD
(Oppositional Defiant Disorder).
Why does this happen?
Like autism, PDA is dimensional and presents differently between individuals, making diagnosis challenging for some children. Characteristics of the PDA profile can overlap with ASD and ODD, leaving interpretation open to human error, like most things in life.
For this reason, a professional may indicate that your child is presenting with Oppositional Defiant Disorder, primarily due to a focus on defiant behaviour.
While autism is a globally recognised diagnosis, our understanding of the autism spectrum and profile subtypes, like PDA, is still evolving.
The PDA testing process
PDA profiling generally forms part of an ASD assessment, undertaken via referral to a PDA-aware child psychologist specialising in autism. You won’t need a referral if your child already has a confirmed ASD diagnosis.
The testing process is collaborative and involves key caregivers in a child’s life, including parents, educators and other relevant professionals.
The assessment phase can vary between clinics, but usually includes the following steps:
Step one is a parent-only appointment to:
- explore your child’s developmental history and skills
- discuss particular concerns and talk openly about challenges
- fill out a take-home a parent/carer questionnaire
Step two is a face-to-face appointment with your child focused on:
- building a relationship and trust
- exploring PDA characteristics through conversation, games and activities that interest them
- using non-directive language to introduce ideas
In this session, we will also explore potential sensory stressors which can assist with profiling and support.
Parents are welcome at face-to-face appointments.
Step three involves seeking feedback from educators and other professionals familiar with your child to explore how they present in a range of environments.
Step four will determine a PDA profile, if appropriate.
Armed with the above information, your child psychologist will apply clinical judgement to diagnose a PDA profile. Younger children who are still developing or don’t fulfil all profile criteria can be diagnosed “at high risk” of PDA.
The testing process can take several weeks and seem daunting at first. Despite this, parents are often relieved by the outcome, as it gives them a better understanding of their child’s needs and a framework for moving forward.
As with all developmental challenges, early testing and identification can improve the quality of life for your child and family.
How to support children with PDA (strategies)
If your child is identified as having a PDA profile, it’s important to remember that you don’t have to navigate this new path alone.
Helping your child control their anxiety is the primary goal of support.
For some parents, the path to effective support begins with a mindset shift. Understanding that your child’s behaviour is driven by anxiety (rather than deliberate behaviour) allows you to better communicate, think ahead and support their needs.
“There is no one-size-fits-all approach to PDA care. Often the strategies we lean on for children with autism can make things worse for children with PDA. Plus, what works well for one child may not work for another, and the effectiveness of strategies can shift over time.”
– Dr Nicole Carvill, Think Psychologists.
The following strategies can be explored and tested in a clinical setting and at home:
- Gently reframe language to be less direct and more conversational. Instead of “I need you to,” use phrases like “I wonder if we can” or “maybe we could investigate”
- Offer a greater sense of control. Allow your child the option to say no or pick between two choices
- Identify the likelihood of sensory overwhelm in upcoming situations and reduce the overwhelm where possible. Consider exploring sensory issues via an OT to reduce uncertainty
- Increase familiarity with situations and tasks to reduce your child’s anxiety
- Keep tasks aligned with your child’s interests where possible
- Think about the length of tasks and activities. Things that take too long to complete may lead to higher anxiety.
Most importantly, be flexible and collaborative with your child when it comes to tasks and expectations. And, if things don’t go as expected, try not to take it personally. Highly anxious PDA kids can make hurtful comments, and this is where reframing is important.
A note for educators:
Keep in mind that building a relationship with a child who has PDA can take time. The child likely has a history of challenging interactions with authority figures, so you must establish trust before working on strategies.

Medication and tools for PDA
Medication to alleviate anxiety can be helpful for some children with PDA. Introducing medicine is a personal choice and one you can explore in collaboration with your child’s psychologist and paediatrician.
Resources and training
Register your interest for our upcoming PDA-aware parenting webinar for parents, or our PDA-aware teaching webinar created for educators, teaching assistants, support workers and therapy assistants.
Expand your knowledge through the PDA Society UK, PDAANZ (Australia and NZ) and follow PDA ambassador The Naughty Autie.

Dr Nicole Carvill is an accomplished child psychologist, researcher, presenter and PhD graduate who dedicates her time to helping children and families thrive. A mother of two and caregiver by nature, she approaches therapeutic support through the lens of a psychologist with the heart of a parent.
